10 Things to Know If Breast Cancer Runs in Your Family
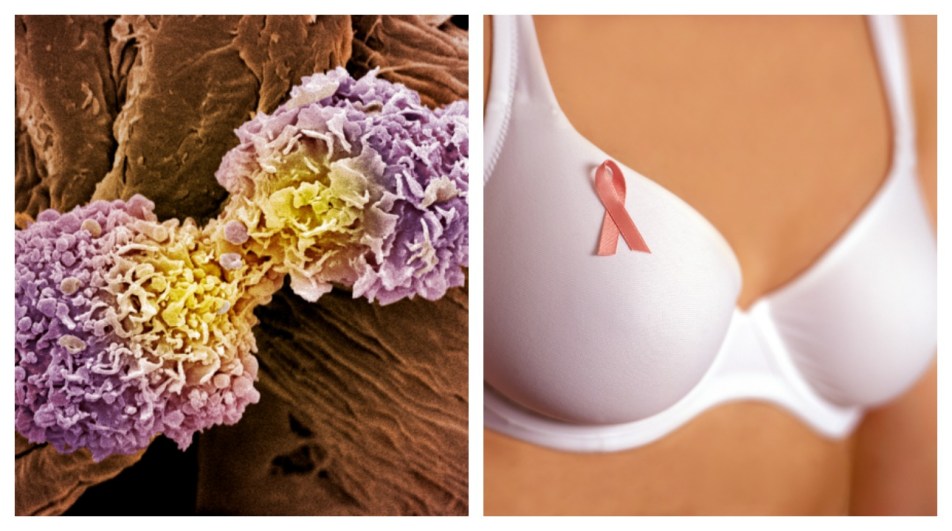
All cancers are caused by genetic mutations, but not all genetic mutations are inherited. When the genes that suppress runaway cell growth don’t function correctly, cells divide uncontrollably and clump together in a tumor. That’s what we call cancer. In most cases of breast cancer, these genes turn faulty because of some environmental factor, like smoking or too much radiation. Other times, though, you inherit a copy from your parents. That’s an inherited mutation.
Hereditary breast cancer only accounts for about 5 to 10 percent of all cancer cases in the U.S., according to the National Cancer Institute. But if you carry the most common genetic mutation (BRCA1), your lifetime risk of developing breast cancer shoots up to about 60 percent. (The average lifetime risk for women is 12 percent.)
To help us sort through the science, we turned to Theodora Ross, M.D., an oncologist and the director of the Cancer Genetics Program at the University of Texas Southwestern Medical Center. But she’s got personal experience along with the professional one. After she was diagnosed with melanoma, she discovered she carried the BRCA1 gene and her risk of developing breast and ovarian cancer was now very high. She wrote A Cancer in the Family: Take Control of Your Genetic Inheritance about her experiences.
Here’s what you need to know to prevent breast cancer if it runs in your family.
Know the odds.
The most common genetic mutations—those in the BRCA1 and 2 genes—account for the majority of inherited cancer cases. The ethnic group that has the highest chance of carrying that mutation is Ashkenazi Jews (those that came from Eastern Europe); they have an 8 to 10 percent chance of having the BRCA1 mutation and a 1 percent chance of having the BRCA2. Non-Jewish Caucasians have a 2 percent chance of carrying both the BRCA1 and 2. But there are other mutations that can elevate your cancer risk. “And we’re finding more and more mutations in new genes associated with inherited breast cancer because the field is evolving so rapidly,” says Dr. Ross.
Look at your entire family tree.
To figure out if breast cancer runs in your family, find out about first and second-degree relatives. First degree includes parents and siblings; second degree includes grandparents, uncles and aunts, nieces and nephews. Third-degree relatives are important (great-grandparents, cousins), but not in the same way as first- and second-degree family members.
Then look for these clues:
A first- or second-degree relative had breast cancer before the age of 50.
A first- or second-degree family member had breast cancer in both breasts.
Don’t exclude your male relatives—or other types of cancers.
The BRCA1 and 2 mutations can cause ovarian, pancreatic, and prostate cancers, as well as melanoma (the most serious skin cancer). So if a first- or second-degree relative has had pancreatic or ovarian cancer or melanoma that’s a sign that breast cancer runs in your family. Another clue: if your dad, uncle, or brother had prostate cancer before age 55.
Don’t be afraid of the truth.
If your family tree is riddled with cancer, you might feel too scared to find out what the odds are for you—or your kids. That’s natural. “I was the queen of denial,” says Dr. Ross. “I was a doctor who’d lost a sister to breast cancer, and almost lost a brother to sarcoma, (a cancer of the soft tissues). And I still didn’t consider the possibility of having a hereditary risk to the disease. It wasn’t until I got diagnosed with melanoma that I went in for testing.” So go to a genetic counselor. (If there’s a good case for the testing, insurance will cover it.) It can save your life—and the lives of your family, says Dr. Ross.
Don’t do DIY testing at home.
Genetic counselors are trained to not only interpret the facts but also calm your fears and recommend the best course of action. Plus, they can provide information in an area that changes quickly—and that’s important.
Be strict about cancer-screening tests.
If you carry a genetic mutation that increases your breast cancer risk, screening every six months is a must.
Then, consider preventative measures.
If you are over 35—and are done having kids (or decided you don’t want them)—you may want to consider what Angelina Jolie did and get your breasts and ovaries removed. That will lower your risk to less than general population (in other words, less than 12 percent). Having your ovaries removed is especially important since there’s no reliable early screening for ovarian cancer.
Keep your drinking in check.
A glass of wine every day may be great for your heart, but it’s not so great if you’re trying to prevent cancer. There’s a strong link between drinking and breast cancer—but how much is too much is still up for debate. Dr. Ross’s take: “A reasonable goal is less than one drink per day.”
Be healthy in other ways.
Eating well and exercising can decrease your cancer risk to a “modest” extent. But just know that even the healthiest person can still get cancer.
Talk to your doctor about hormone replacement therapy.
A new study came out with an alarming statistic: Combined hormone therapy (estrogen plus progesterone) could triple a woman’s risk for breast cancer. Dr. Ross’s take: There’s no risk when the hormone therapy only includes estrogen. But to be safe, talk to your doctor about the risks and benefits.


















