If You Suffer From Urinary Leaks, Unexplained Constipation and/or Painful Sex, You Could Have This Sneaky Pelvic Problem
40% of all women will suffer from pelvic organ prolapse — here's what doctors want you to know

When you envision the complicated inner machinery in women’s bodies — and all the pushing and pulling that goes on with pregnancy and childbirth — it’s no surprise that as the years roll by and gravity takes its toll, the positioning of the pelvic organs (especially the uterus, bladder, rectum) could easily get out of whack. And it will for almost half of women globally. Pelvic organ prolapse (POP) is the surprisingly common condition that no one talks about. It happens when one or more of the pelvic organs (including the uterus, bladder and rectum) become too weak to support the pelvic organs, so they drop from their normal position into the vagina. For some women, this happens all at once and feels almost like ball dropping into the vagina or a tampon sliding down too low; but for others, the signs are more subtle and include unexplained constipation and/or feelings of discomfort during sex.
Pelvic organ prolapse symptoms are so variable (and often so personal) that they often get missed by doctors. That’s what happened to Mary Pippen, 59, who suffered from unexplained constipation and a sense of pressure (both common pelvic organs symptoms) in her vagina for years before something happened that was so dramatic, doctors had to pay attention. (Keep scrolling for her complete story.)
We talked to ob/gyns, urogynecologists and pelvic floor specialists to learn more about the four different kinds of POP. Read on for the experts’ take and then keep scrolling for one woman’s story of healing.
What is pelvic organ prolapse?
“Pelvic organ prolapse occurs when the pelvic musculature, which supports the uterus, bladder and rectum, are weakened, causing the organs to drop and press into or out of the vagina,” explains Kecia Gaither, MD, FACOG, double board-certified in ob/gyn and Maternal Fetal Medicine, Director of Perinatal Services/Maternal Fetal Medicine at NYC Health + Hospitals/Lincoln in the Bronx.
Pelvic organ prolapse will affect 40% of women at some point in their life, according to research in the journal Frontiers in Public Health, and the risk rises with age, as body tissues get lax. Pelvic organ prolapse is most likely to strike between the ages of 60 and 69. That said, the most common initiating causes are pregnancy and childbirth. Other factors like family history, hormonal changes during menopause, obesity, chronic coughing, or straining during bowel movements may also contribute to pelvic organ prolapse, according to Dr. Gaither.
Why is pelvic organ prolapse so underdiagnosed?
A complicated interconnecting group of factors contribute to both medical practitioners and women themselves being unaware of the condition. These include
- Cultural and societal taboos: Many of the symptoms of POP involve pain and discomfort during sex, which women are hesitant to bring up their doctors and doctors are hesitant to initiate discussions around. In general, pelvic health issues, like POP, are often cloaked in shame and stigmatized in many cultures around the world.
- Gender bias in medicine: Women’s health issues have been less researched and emphasized compared to the medical concerns of men. Most clinical studies involve younger people and men preferentially.
- Symptoms overlap with other conditions: The four different kinds of POP have four different sets of symptoms — many of which are common symptoms. That makes it harder for doctors and women themselves to recognize and report.
- Variability in severity: For many women with POP, the symptoms are so mild that they don’t require treatment — at least not at first.
- Specialty divides: Management of POP often falls between the specialties — gynecology, urogynecology, or general surgery — depending on the exact nature of the prolapse. This happened for Mary Pippin: Her gynecologist at first dismissed her symptoms. It wasn’t until she visited a urogynecologist that she found her cure.
The four types of pelvic organ prolapse
Depending on the pelvic organ affected, your doctor may diagnose you with one (or more) of the following types of pelvic organ prolapse:
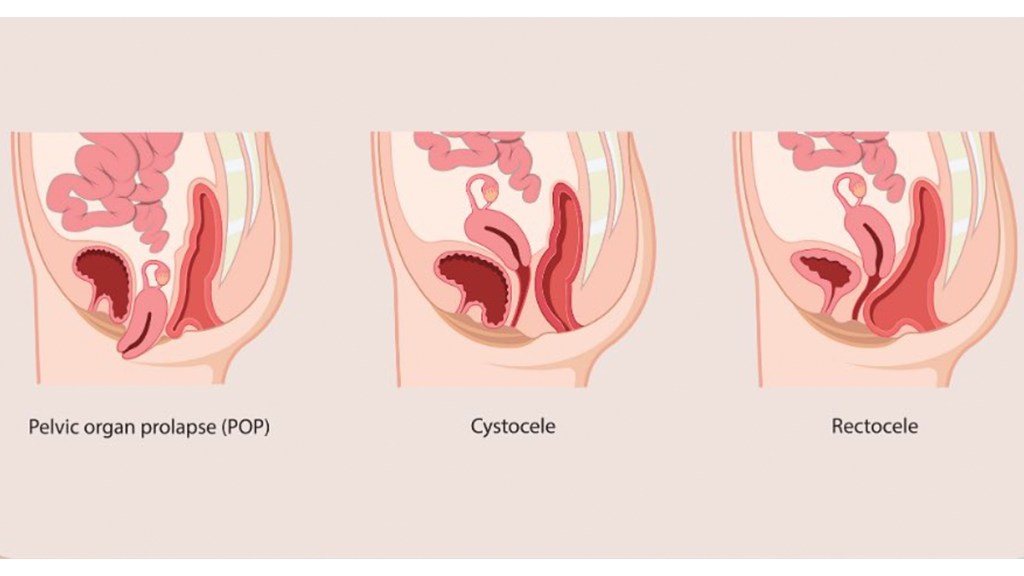
Uterine prolapse: More common in women who have given birth, this occurs when the uterus descends into the vaginal canal.
Cystocele: Also called an anterior prolapse, this happens when the bladder drops into or out of the vagina.
Rectocele: Also called a posterior prolapse, a rectocele involves the rectum bulging into the back wall of the vagina.
Enterocele: Also called small bowel prolapse, this involves the small intestine pushing against the upper vaginal wall.
Symptoms of pelvic organ prolapse
Aldene Zeno, MD, FACOG, a double board-certified ob/gyn and urogynecologist at Essence Health and Urogynecology, says a common symptom includes a vaginal bulge, which patients often describe to her as a “ball” sensation. “Some of my patients describe feeling like something is ‘out of place,’ like a tampon that’s too low, which makes sense because the upper part of the vagina doesn’t sense pain in the same way that the lower two-thirds of the vagina does,” she explains.
Although prolapse is rarely painful, Dr. Zeno says it can cause a feeling of pressure that worsens over the course of the day or during certain movements like squatting, bending over, or lifting something heavy. “Patients are more likely to describe a pulling, tugging, or cramping sensation like menstrual cramps, as opposed to severe pain, though it is possible,” she explains.
Dr. Zeno says you may also experience additional symptoms depending on which organ is prolapsed:
Additional uterine prolapse symptoms
In addition to the bulge and other symptoms above, women experience:
- Increased need to urinate
- Feeling like you need to empty your bladder when you already have
- Painful intercourse
Additional rectocele symptoms
When the rectum is more involved, Dr. Zeno says you may experience difficulty evacuating your bowels, which can lead to straining and constipation or the opposite, with accidental bowel leakage. Rectal pain is also common, as is painful intercourse, vaginal bleeding and a feeling of fullness in the vagina. (Click through to read more about the link between constipation and back pain, and how to get relief.)
Additional cystocele symptoms
“If the bladder is more involved, patients may experience a sensation to urinate frequently or have bladder leaks,” says Dr. Zeno. In extreme cases, she says the bladder can become difficult to empty, which can cause frequent bladder infections or urinary retention, or an inability to empty all the urine from your bladder, which is an emergency situation. (Click through to learn about meds that cause bladder leaks.)
Additional enterocele symptoms
Women with enterocele may not actually experience any symptoms, but in more advanced cases, women will experience a vaginal bulge or feelings of pressure, long with painful intercourse and lower back pain that gets better when they lie down.
How doctors diagnose pelvic organ prolapse
If you have symptoms of pelvic organ prolapse, Dr. Zeno recommends seeing a qualified clinician, typically a general ob/gyn or specialist called a urogynecologist, for a diagnosis. During that visit, Dr. Zeno says the clinician will do a pelvic exam similar to a Pap test, but a specialist should be able to tell which vaginal compartments are falling the most. “They can see if the vaginal walls most involved are in the front/bladder, top/uterus (if present) or back wall/rectum,” she says.
Treatment is warranted if the symptoms are bothersome, which doesn’t just mean physical discomfort. Some women also experience issues with sexuality and body image that may be alleviated with the right treatment.
Nonsurgical treatment options for pelvic organ prolapse
Before considering surgery, your doctor may discuss nonsurgical options. A few methods that can help:
Pessary for pelvic organ prolapse
“A pessary is a medical device typically made of silicone that is fitted during a clinical pelvic exam with a gynecologist,” says Dr. Zeno. Once you have the correct shape and size, Dr. Zeno says you may be able to take care of it yourself by placing and removing it. But if your prolapse is more advanced, your doctor may recommend a pessary that has to be placed and removed by your doctor, she says.
One caution for postmenopausal women, who may experience complications due to the natural thinning and drying of the vaginal skin. “For my postmenopausal patients, I typically recommend they also use vaginal estrogen to improve the vaginal tissue quality because there are risks with the pessary that involve damage to vaginal tissue over time.” (Click through for more ways to treat vaginal dryness)
Kegels for pelvic organ prolapse
If you’ve gone through pregnancy and childbirth, you’re likely a pro at Kegels, especially since most of us remember our doctors telling us to do them literally everywhere — at a stoplight, in line at the store, or while watching TV.
That’s because Kegel exercises specifically target the pelvic floor muscles, which act like a hammock to support the pelvic organs. Strengthening these muscles can provide better support to the organs, and research shows they can even improve symptoms of pelvic organ prolapse,
Here’s a quick how-to for getting started with Kegel exercises:
- Identify your pelvic floor muscles by stopping the flow of urine midstream. Those are the muscles you want to target.
- Sit, stand, or lie down in a comfortable position. You can do Kegels anywhere, anytime without anyone knowing.
- Contract the Muscles: Squeeze your pelvic floor muscles for about 3 seconds, then relax for 3 seconds. Gradually increase the duration as your muscles get stronger. If you’re unsure how to do this, think of squeezing the muscles you use to stop the flow or urine. You should feel a contraction that pulls the vagina and rectum up and back.
- Breathe: Don’t forget to breathe. Inhale as you relax, and exhale as you squeeze.
- Repeat: Aim for three sets of 10 repetitions per day.
Here’s a helpful video to help you get started:
Pelvic floor physical therapy for prolapse
Beyond Kegel exercises, Dr. Zeno says pelvic floor physical therapy can help offload the pelvic floor and improve muscle movements during activities like lifts, bends and squats. There are several online programs available, though Dr. Zeno recommends in-person evaluation and treatment with a pelvic floor physical therapist.
She also says reducing constipation can help alleviate the chronic pressure that strains the pelvic floor and worsens prolapse. “There’s some evidence that these treatments are especially beneficial in women with early-stage prolapse, and in some cases, the prolapse can actually improve over time (after 6 to 12 months),” she explains. Click through for 3 exercise poses for prolapse from pelvic health specialist Trista Zinn to lift and strengthen the pelvic floor, correcting prolapse. And click here to read about the benefits of pelvic floor massage.
Surgical treatments for pelvic organ prolapse
If pain or discomfort significantly interferes with daily life, your doctor may recommend either obliterative or reconstructive surgery. Obliterative surgery, which is often called a colpocleisis, involves narrowing or closing off the vagina to provide support. It has a high success rate but is not recommended for women who are sexually active or want to continue to have sexual intercourse.
Reconstructive surgery involves restoring the organs to their original position, which is the way to go if you’re still sexually active. There are several types of reconstructive surgery, and Dr. Zeno says most are minimally invasive and rarely involve large incisions on the belly. Instead, they are typically done either vaginally (no abdominal incisions) or by laparoscopy.
“Most of my patients go home the same day with prolapse surgery, and since the surgeries are relatively low-risk, even patients with pre-existing health issues can safely undergo surgery,” she says.
Pelvic organ prolapse success story: Mary Pippen

Yikes! What is that? Mary Pippen wondered as she froze in her tracks. She was in the middle of a training session for a triathlon when her body suddenly felt…off. “It felt like something fell in my vagina — like a tennis ball was trying to push its way out,” she recalls. “I had to grab my bottom and push back whatever had dropped inside me. I thought I’d need to have someone call 911 because I didn’t have my phone with me. But as I stood there and nothing else happened, I realized it wasn’t a life-threatening situation. I wasn’t in pain or bleeding, I didn’t feel like I was going to pass out — there was just a strange pressure.”
“I walked home, Googled it, and figured out that the problem was with my uterus. It hadn’t come all the way out — it was just poking out an inch or so — so I called my gynecologist. The nurse assured me this wasn’t an emergency and scheduled me to see the doctor two days later. During those 48 hours I was scared and uncomfortable, to say the least.”
“At the exam, the gynecologist diagnosed me with uterine prolapse cystocele, which means my bladder bulges into my vagina, and rectocele, which means my rectum bulges into my vagina. He explained these conditions to me, and when I seemed surprised, he said, ‘What did you expect? You’re 50, you’ve had four kids, and you run.’ He basically told me to live with it. I didn’t know how to respond. At the time, I didn’t know what prolapse was — I didn’t even know enough about the female body to know what to ask. Honestly, I just wanted to get out of there. So I went home, and whenever my uterus dropped, I would just push it back up and go about my business.”
Mary thought she had to just live with her symptoms
“Looking back, I’d had some symptoms that I either ignored or reported too vaguely. In 2004, I started having trouble with constipation: I’d start a bowel movement and it would get stuck, so I’d strain. I told my doctor I was constipated, but I didn’t describe the stuck sensation; she told me to eat more fiber and drink a lot of water, which I was already doing. So I started popping laxatives once a week. In 2012, I stopped being able to wear a tampon — it would slide, which was hard because I was going through perimenopause and my periods were all over the place.”
“Plus, over time, I had lost sexual sensation and my ability to have an orgasm. I later found out this was related to the prolapse, but at the time I didn’t understand it — I thought it must be psychological. It made me lose interest in sex, which was hard on my marriage. I went into a deep, dark depression before the diagnosis. I felt gross and unwell and unsexy.”
The surgery that changed Mary’s life
“A few months after I received the diagnosis, I found the Association for Pelvic Organ Prolapse Support (APOPS) and went to a urogynecologist who diagnosed me with stage three uterine prolapse, told me a lot more about it, and advised surgery. I had a laparoscopic hysterectomy with vaginal vault suspension to support my bladder and the other remaining organs. After surgery, I took six weeks off from work, and I did physical therapy to strengthen my pelvic floor. Honestly, I was fine with having a hysterectomy; I had no emotional ties to my uterus, and I was happy not having any more periods.”
“Unfortunately, a few months later, my bladder fell, and I had to have another procedure to secure it back in place. I still have the rectocele, but it’s manageable — I make sure I have enough fiber and water, and I take magnesium citrate supplements and Miralax (Buy on Amazon, $26.35 for 45 doses, Amazon) on occasion, to keep my bowel movements regular and soft enough to pass without straining.
Today, Mary feels stronger and healthier
“At the physical therapist’s urging, I stopped running and instead, I work out in the gym several times a week. I also walk, hike, swim, bike, play pickleball and do pretty much any activity I want to do. Prolapse robbed me of being able to do triathlons and play tennis, both of which my family would do with me. I miss those activities, but I’m not willing to risk going back to where I was with this condition.”
“On the upside, sex is awesome again. I can have orgasms and my libido is back. And I generally feel much more comfortable. One of the things I learned with physical therapy is how to feel vaginal pressure and figure out what doesn’t feel right. It’s amazing — this condition has been going on since B.C. yet it isn’t talked about. It turns out my mom had prolapse, but she didn’t tell me about it! And while I do hate pelvic organ prolapse, I’m also grateful for it because after going through this journey, I’ve become a more empathetic, stronger woman. I’m now an admin for the APOPS support forum on Facebook so I can help other women reclaim their health!”
This content is not a substitute for professional medical advice or diagnosis. Always consult your physician before pursuing any treatment plan.
For more stories on menopausal health bothers, keep reading:
“Perimenopause Made Me Foggy and Tired — Until I Found This Natural Cure!”
Gynecologists Break the Silence On ‘Hair Down There’ Over 50 — All Your Questions Answered The 9 Best Foods That Fight Hot Flashes, According to MDs — No Medication Required













